|
Management of Common
Coccydynia
Jean-Yves Maigne, MD, Paris, France |
Visit our special section devoted to coccydynia
Common
coccygodynia is poorly understood. Numerous hypotheses have been proposed as to
the origin of the syndrome, including pain from the pericoccygeal soft tissues,
spasm of the muscles of the pelvic floor, referred pain from lumbar pathology,
arachnoiditis of the lower sacral nerve roots, local posttraumatic lesions,
somatization, etc (Howorth 1959, Jurmand 1976, Nelson 1991, Postacchini and
Massobrio 1983, Stern 1967). Thus far, there has been no sound confirmation of
any of these.
Because patients often mention a fall on the buttocks or a delivery as
precipitating event, a mechanical basis for the pain is likely. In addition, in
the majority of cases, the pain occurs only in the sitting position. These
factors led us to develop a protocol to document the painful coccyx with dynamic
films and coccygeal discography (Maigne et al 1992, 1994). Dynamic films are
defined as X-rays films in the lateral sitting position (the painful position)
as compared with standard lateral roentgenograms. Since 1992, more than 700
patients with coccygeal pain have undergone this protocol. We summarize here the
results of our studies on this topic.
|
|
|
Anatomical study of
the sacrococcygeal and intercoccygeal discs
|
|
|
There is a
paucity of information regarding this topic. According to Gray (1973), the
sacrococcygeal joints are thin intervertebral discs of fibrocartilage.
Occasionally, the intercoccygeal joints are synovial.
By examining nine aged coccyges from fresh cadavers, we found that the
sacrococcygeal joint was a disc in one case, a synovial joint in four cases and
a third type in four cases, the joint being an intermediate structure made of a
disc containing a more or less extensive cleft, parallel to the end plates, and
bordered by annular fibres or synovial cells (Maigne et al 1992). This
intermediate state was not found in the intercoccygeal joints. It is not known
if young individuals show the same distribution or not, i.e. if a sacrococcygeal
joint can be transformed from one form to another during a person's lifetime.
A fourth type exists, in the form of ossification. Ossification can involve only
the sacrococcygeal joint. Studying two different populations, the frequency of
this type was found in 22 and 68% of the cases by Saluja (1988). In some of our
patients, the whole coccyx was ossified.
The physiologic movements of the coccyx are restricted to flexion and extension.
Active flexion (movement in a forward direction) is performed by the levator ani
and the sphincter ani externus muscles. Extension (movement in a backward
direction) is due to relaxation of these muscles and to the increased
intra-abdominal pressure which occurs during defecation and parturition (Smout
1969). It is a passive movement. Surprisingly, the movements of the coccyx in
the sitting posture have never been reported in the literature to our knowledge.
Flexion or extension can be encountered. Passive flexion is due to the direct
pressure of the seat over the coccyx. In other cases, a passive extension is
encountered, which is due to an increased intra-pelvic and abdominal pressure by
the seat. The direction is depending on the coccygeal anatomy. The intervening
factors are : 1) The angle between the sacrum and the coccyx (an acute angle
makes the coccyx prone to flex, a flat angle makes it more prone to extend). 2)
The sagittal pelvic rotation when sitting (a high degree of pelvic rotation when
sitting brings the coccyx parallel to the seat, leading to flexion, a low
rotation let it more or less vertical, prone to extension). 3) The body mass
index, which is closely related to the pelvic rotation and 4) The angle of
coccygeal incidence, which is also related to the pelvic rotation (see below).
In other cases, the coccyx is not mobile when sitting (more frequently in
males). This may sometimes (but not always) be attributed to a joint
ossification.
|
|
|
Technique of
dynamic films
|
|
|
The standard way
to X-ray the coccyx is to take the film in the standing position. I coined the
word "dynamic exploration" for the comparison between a
standard film and a "dynamic film", in a sitting (painful) position. The first
(standard) film is taken in the lateral standing position. In order for the
coccyx to be in a neutral position, it is very important for the patient to
avoid sitting for the five to ten minutes preceding the X-rays examination.
Otherwise, in some cases of hypermobility or luxation, there is not time enough
for the coccyx to come back into the neutral position. The second (dynamic) film
is taken laterally while asking the patient to sit on a hard stool with the back
slightly extended from a sitting position, in a posture in which the pain is
most pronounced (figure 1). It is mandatory to wait a few minutes for the pain
to occur. If the pain is not present, no sound conclusion should be drawn.

Figure 1. The correct position to X-ray the coccyx in a
sitting posture. Note the foot rest.
Both films are superimposed on a bright light in order to compare and measure
movement of the coccyx. The shapes of the two sacrum should correspond exactly,
in order to evidence the coccygeal mobility. Only its mobile portion is
considered, the saccrococcygeal disc being sometimes ossified or not mobile.
This movement is measured in degrees of flexion or extension (figure 2).
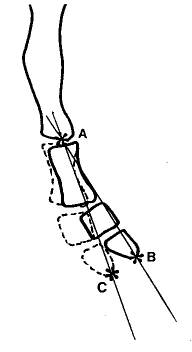
Figure 2. Range of motion of the coccyx is measured in
degrees (angle ABC). Bold line: standard film. Dotted line : coccyx in the
sitting position. A: apex of the angle located at the caudal part of the sacrum
(or of the first coccygeal vertebra if the sacro-coccygeal disc is ossified).
The subject is facing to the right, the opposite of figure 1.
In a first study (Maigne et
al 1994), the films of 51 patients and controls were compared and read by two
independent observers at two different time intervals, the second reading
performed one month later. The final value used was the average of the four
separate readings. Inter- and intraobserver variations of the angle measurement
were 12.5% and 15.3% respectively, and the accuracy of the measurement technique
was +/- 2.6 degrees. This is therefore a reliable technique, in particular in
view of the definition of hypermobility (see below).
|
|
|
Mobility of the
normal coccyx
|
|
|
In a
control group consisting of 47 pain free volunteers with no history of local
trauma and no more than two pregnancies (Maigne et al 1994), the mean mobility
(flexion or extension) was 9.3+/-5.7 degrees (range from 0 to 22 degrees).
Thirteen coccyges (27.6%) had an extension between 5 and 15 degrees and eight
(17%) a flexion between 5 and 22 degrees. Twenty-four (51%) others had a very
limited mobility between 0 and 5 degrees. In two cases, there was a slight
(asymptomatic) backward slipping of less than 20% (one fifth of the AP diameter
of the vertebra).
Allowing for a certain degree of non pathologic variation, we therefore consider
that flexion larger than 25-30 degrees represents hypermobility and slipping
larger than 25% represents luxation. Extension larger than 15-20 degrees is also
pathologic, but it is a very rare situation.
Whether coccyges flex or extend in the sitting position (in controls and in
patients) is based upon their position related to the horizontal plane of the
seat at the very moment when the pelvis reaches the seat. If the coccyx is near
a vertical position (related to the seat), the increase of the pelvic pressure
will push it backward (extension). However, if the coccyx is near the horizontal
position (i.e. parallel to the seat), the pelvic pressure will have no effect on
it. It is the direct pressure exerted by the seat which pushes it forward (into
flexion). The angle between the mobile coccyx and the horizontal is the
coccygeal incidence. An approximate value of this angle can be calculated on the
dynamic film (figure 3). If this angle is larger than 35 degrees, the coccyx is
likely to extend when sitting. Under 12 degrees, it will flex. Between 12 and 35
degrees, 61% of the coccyges had flexion, and 39% extension in our study (Maigne
et al, 1996).
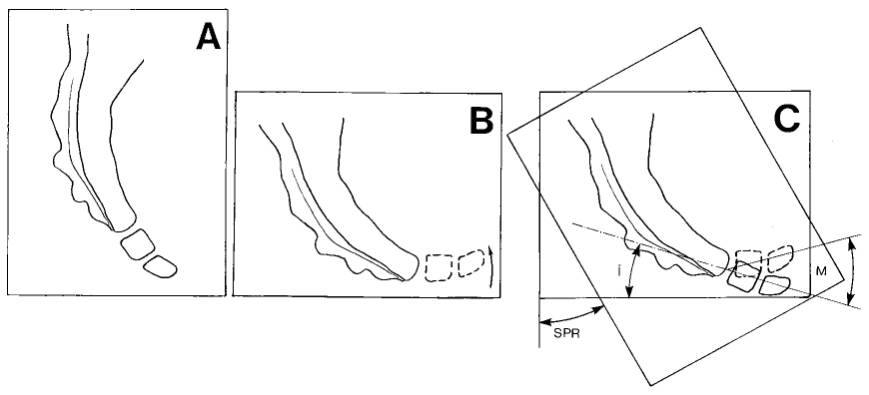
Figure 3. Measure of the coccygeal incidence. A: standing
film. B : sitting film, showing a normal flexion. C: measure of the angle (i);
this angle reflects the theoretical position that the mobile part of the coccyx
would take if the subject was "sitting without the seat", that is without any
force acting on it. M = coccygeal mobility, the angle by which the coccyx has
rotated relative to the sacrum. SPR = saggital pelvic rotation, the angle by
which the pelvis has rotated in going from standing to sitting.
|
|
|
The coccyx in
common coccydynia: radiologic lesions
|
|
|
Standard and
lateral sitting radiographs of more than 700 patients suffering from common
coccygodynia for at least 2 months duration have been made since 1992. Four
series of different patients have been currently published, allowing some firm
conclusions on the pathology of the coccyx.
 Posterior luxation and
subluxation: Sagittal luxation of all or part of the mobile portion of
the coccyx while in the sitting position is the most striking abnormality
observed (figure 4). It is noticed in 20 to 25% of the cases. The sacrococcygeal
disc and the first intercoccygeal disc are equally affected. This luxation is
spontaneously reduced in the standing position. In some very rare cases, it is
permanent. Posterior luxation and
subluxation: Sagittal luxation of all or part of the mobile portion of
the coccyx while in the sitting position is the most striking abnormality
observed (figure 4). It is noticed in 20 to 25% of the cases. The sacrococcygeal
disc and the first intercoccygeal disc are equally affected. This luxation is
spontaneously reduced in the standing position. In some very rare cases, it is
permanent.

Figure 4. Luxation of the
first mobile vertebra in the sitting position (right). Standard film on the
left. The subject is facing to the left, as in figure 1.
Such a lesion is
never observed in pain free controls and there is no doubt about its role in
coccydynia.
Patients with luxation have certain characteristics, which set them apart from
those with normal dynamic films. Their Body Mass Index is statistically higher.
A history of direct and violent traumatism on the coccyx prior to the pain is
more often found. An acute pain while passing from the sitting to the standing
position, more intense than the usual pain felt in the sitting position, is also
frequently found.
 Hypermobility in
flexion: Hypermobility is defined by flexion of the coccyx of more than
25-30 degrees in the sitting position (figure 5). It is found in 20 to 25% of
the cases. The extreme and mean values in this subgroup is 25-70 and 35 degrees
respectively. Hypermobility always occurs in flexion, and almost never in
extension. Hypermobility in
flexion: Hypermobility is defined by flexion of the coccyx of more than
25-30 degrees in the sitting position (figure 5). It is found in 20 to 25% of
the cases. The extreme and mean values in this subgroup is 25-70 and 35 degrees
respectively. Hypermobility always occurs in flexion, and almost never in
extension.
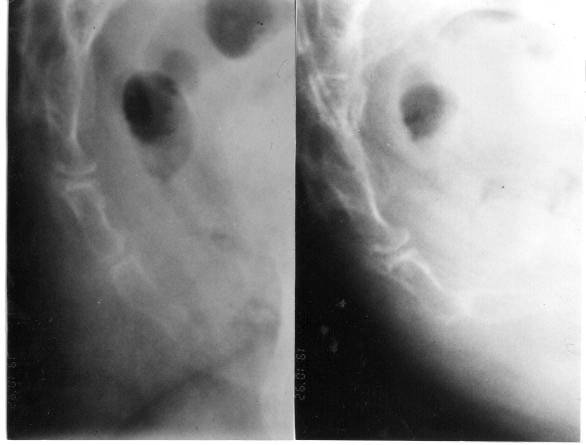
Figure 5. Hypermobility. On the left, standard film. On
the right, film in the sitting position, with the last joint of the coccyx lying
horizontal. Subject is facing to the right.
Mild hypermobility (25-35
degrees) can also be found in patients with hyperlaxity joint syndrome. It is
not always a painful abnormality.
Luxation and hypermobility can be interpreted as coccygeal instability similar
to lumbar instability. It is of interest that contrary to the degenerative
lumbar disc, the coccygeal disc does not sustain any compressive load which
would lead to osteophytes formation, considered to act as restabilizing
processes.
 Coccygeal spicule:
We have described an abnormality in the form of a small bony
excrescence on the dorsal aspect of the tip of the coccyx, involved in 15% of
the cases of coccydynia. We termed it a 'spicule'. When it is present, it can
always be readily palpated, jutting out under the skin; it would cause
irritation on sitting. Interestingly, in 70% of the cases, there is a pit of
greater or lesser depth in the skin overlying the spicule. This pit is usually
fairly discreet, but in some cases, it is a frank retrococcygeal pilonidal sinus
(without any discharge or abscess). We consider the pit to be evidence of the
embryonic origin of the malformation (figure 6). These spicules are most
commonly seen in non mobile coccyges, in which the pressure from the spicule is
made worse by the inability of the coccyx to take evasive action. Coccygeal spicule:
We have described an abnormality in the form of a small bony
excrescence on the dorsal aspect of the tip of the coccyx, involved in 15% of
the cases of coccydynia. We termed it a 'spicule'. When it is present, it can
always be readily palpated, jutting out under the skin; it would cause
irritation on sitting. Interestingly, in 70% of the cases, there is a pit of
greater or lesser depth in the skin overlying the spicule. This pit is usually
fairly discreet, but in some cases, it is a frank retrococcygeal pilonidal sinus
(without any discharge or abscess). We consider the pit to be evidence of the
embryonic origin of the malformation (figure 6). These spicules are most
commonly seen in non mobile coccyges, in which the pressure from the spicule is
made worse by the inability of the coccyx to take evasive action.
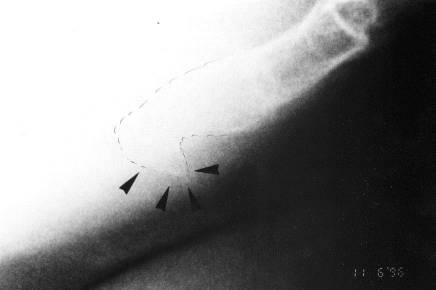
Figure 6. Coccygeal spicule.
Spicules are implicated in
the causation of coccydynia on the following evidence:
1. spontaneous, non-trauma-related onset of the coccydynia, as commonly seen in
inflammatory lesions
2. pain felt at the tip of the coccyx (unlike the pattern seen with the other
coccygeal lesions, where the pain is greatest at the level of the joint
involved) and elicited very precisely by pressure on the spicule (which is
always readily palpable under the skin)
3. visualization of the bony excrescence with imaging techniques
4. pain relief following local anaesthesia.
 Coccyges without
radiologic abnormality: In 40% of the cases, the dynamic exploration
fails to demonstrate a lesion. These cases with normal dynamic films represent
the actual "idiopathic" coccydynia. The pain may be related to different
problems. Coccyges without
radiologic abnormality: In 40% of the cases, the dynamic exploration
fails to demonstrate a lesion. These cases with normal dynamic films represent
the actual "idiopathic" coccydynia. The pain may be related to different
problems.
· Intradiscal inflammation. Some of these patients respond well to an
intradiscal (coccygeal) injection, making likely a diagnosis of chronic joint
inflammation.
· Chronic bursitis. In case of a rigid coccyx, with pain located at the tip,
even without spicule, a bursitis is possible. Injection of the subcutaneous
tissues with anaesthetic may suppress symptoms, thus confirming the diagnosis.
· In some cases, the pain is located at the sacral insertion of the
sacrotuberous ligament. This could be compared to a local sprain, and treated
with steroid injections.
· Psychogenic pain ('hysteria', neurotic pain or depression) was formerly
considered as a common aetiology. In our different series, we have considered
this diagnosis in only a very few cases. The main feature is a permanent pain,
not enhanced by sitting, which is fairly abnormal in coccydynia.
· Pain referred from other structures is another possibility. The sacroiliac
joint or the lumbosacral area are sometimes advocated as a possible origin of
coccydynia. These diagnosis should be evoked only if the coccyx appears normal
after the dynamic exploration.
Whatever the lesion observed on the dynamic films, palpation over the coccygeal
area should demonstrate tenderness corresponding precisely to the 'pathologic'
level (i.e. coccygeal disc). The other level should not be tender. When there is
no obvious lesion on the films, careful palpation is the only way to determine
the tender level, deemed to be the responsible level. This is specially
important if a treatment by intradiscal injection is considered.
|
|
|
Treatment of common
coccydynia
|
|
|
Three methods can
be used: manipulation, injection or surgery (coccygectomy).
 Manual treatments:
Manual treatments consist in either manipulations of the coccyx or
massages of the pelvic muscles (levator ani or piriformis). This is a very
classic treatment of coccygeal disorders. In an open study by Wray et al, adding
manipulation to injection treatment produced a 25% increase in the rate of
satisfactory results. Manual treatments:
Manual treatments consist in either manipulations of the coccyx or
massages of the pelvic muscles (levator ani or piriformis). This is a very
classic treatment of coccygeal disorders. In an open study by Wray et al, adding
manipulation to injection treatment produced a 25% increase in the rate of
satisfactory results.
Massages of the pelvic floor were described by Thiele (1937). Manipulations
consist in mobilisations of the coccyx in joint mobilisation and stretching of
the coccyx (and of the attached muscles) with the rectal finger. This latter
manoeuvre was described by R Maigne (1961). We have designed a personal
technique, consisting in a mild levator and external sphincter stretch without
moving the coccyx (Maigne et al, 2001).
These three
techniques have been compared in a prospective pilot study (Maigne
et al, 2001). Patients were randomized into three groups, each of which
received three to four sessions of one of these three different treatments (levator
ani massage, joint mobilization, mild levator stretch). Assessment with a visual
analog scale was performed by an independent observer, at seven days, 30 days,
six months, and two years. Results of the manual treatments were satisfactory in
25.7% of cases at six months, and in 24.3% at two years. Results varied with the
cause of the coccydynia. Patients with a rigid coccyx did least well; we assume
that the reason is that the cause for pain is inflammatory in nature (spicule or
bursitis). Those with a normally mobile coccyx did best. This could be because
one reason for the pain could be a spasm (or at least a painful tension) of the
levator ani. Patients with luxation or hypermobility had in-between results
(more important was the pain intensity, poorer were the results). Levator ani
massage and stretch were more effective than joint mobilization, which worked
only in patients with a normally mobile coccyx. Pain when standing up from
sitting, and excessive levator tone, were associated with a good outcome.
However, none of the results was significant, because of the low success rate of
manual treatment.
There is a need for a placebo-controlled study, to establish conclusively
whether manual treatments are effective. This study is current in our
department. To date (2001-12-01), 80 patients have been enrolled.
 Injections:
The technique of coccygeal discography is simple. It is conducted under
fluoroscopic guidance. The patient is asked to lie on his/her left side with the
hips flexed. The skin is carefully disinfected. The responsible disc (to be
injected) is selected under the following criteria: radiologic abnormality
(luxation or hypermobility) and/or tenderness at this level. When a spicule is
responsible, there is no need to inject a disc, but the spicule itself. Injections:
The technique of coccygeal discography is simple. It is conducted under
fluoroscopic guidance. The patient is asked to lie on his/her left side with the
hips flexed. The skin is carefully disinfected. The responsible disc (to be
injected) is selected under the following criteria: radiologic abnormality
(luxation or hypermobility) and/or tenderness at this level. When a spicule is
responsible, there is no need to inject a disc, but the spicule itself.
Each disc or
synovial joint is entered with a 25g, 25mm needle under aseptic conditions,
using a posterior approach through the midline, to avoid small blood vessels. We
inject a very small amount of dye to control the position of the needle and a
steroid (figure 7). The injection is generally effective within one week. In
case of partial relief, another injection can be done one month later. The
abnormal mobility, if present, remains, but ceases to be painful.

Figure 7. Coccygeal discography. The figure shows a
synovial joint.
In our 1996 study (Maigne et
al, 1996), we have established that patients with luxation or hypermobility were
better responders to a local intradiscal corticosteroid injection than patients
with normal coccyges. About two months after the injection, 50% of the patients
with luxation or hypermobility were improved or healed, whereas only 27% of the
patients with normal coccyges improved. The difference is significant (Chi
square = 4.53, p = 0.033). In case of relapse, a second injection may be
performed. If the result is better after this second injection (a longer
relief), the prognosis is good. If the relief is shorter, injections do not
appear to be the right treatment. Usually, spicule do very well after one or two
injections.
Another treatment for unstable coccyges could be prolotherapy. Although I have
no experience in this method, the rationale for its use is interesting (Dorman,
personal communication, 1995).
 Surgical
coccygectomy: Coccygectomy is a controversial subject. Some authors
have reported good results; however, selection criteria are ill-defined. Others
advise against this procedure. Pyper stated that 'there is no constant factor in
the history, no reliable physical sign, and no specific radiographic change that
can be regarded as a definite pointer in advising operation' (Pyper, 1957). We
have published a study to validate an objective criterion for patient selection:
radiological instability of the coccyx (intermittent luxation, or hypermobility
of the coccyx). We have enrolled prospectively 37 patients with chronic
coccygodynia due to coccygeal instability (intermittent luxation, or
hypermobility) unrelieved by conservative treatment, and not involved in
litigation. The operation was performed by the same surgeon (L Doursounian).
Patients were followed up for a minimum of two years after coccygectomy, with
independent assessment at two years. There were 23 excellent and eleven good
(91%), and three poor results. This appear to be one of the best results of the
literature. The average time to definitive improvement was 4 to 8 months, which
is fairly long, but in line with other authors' reports. Such a long interval of
time could be explained by a 'phantom limb syndrome', coccygectomy being an
amputation. When improvement is slow to appear, we prescribe amitriptyline,
which seems to help. Surgical
coccygectomy: Coccygectomy is a controversial subject. Some authors
have reported good results; however, selection criteria are ill-defined. Others
advise against this procedure. Pyper stated that 'there is no constant factor in
the history, no reliable physical sign, and no specific radiographic change that
can be regarded as a definite pointer in advising operation' (Pyper, 1957). We
have published a study to validate an objective criterion for patient selection:
radiological instability of the coccyx (intermittent luxation, or hypermobility
of the coccyx). We have enrolled prospectively 37 patients with chronic
coccygodynia due to coccygeal instability (intermittent luxation, or
hypermobility) unrelieved by conservative treatment, and not involved in
litigation. The operation was performed by the same surgeon (L Doursounian).
Patients were followed up for a minimum of two years after coccygectomy, with
independent assessment at two years. There were 23 excellent and eleven good
(91%), and three poor results. This appear to be one of the best results of the
literature. The average time to definitive improvement was 4 to 8 months, which
is fairly long, but in line with other authors' reports. Such a long interval of
time could be explained by a 'phantom limb syndrome', coccygectomy being an
amputation. When improvement is slow to appear, we prescribe amitriptyline,
which seems to help.
Thus,
coccygectomy gives good results in a subset of patients with instability of the
coccyx. This objective criterion (instability of the coccyx) should replace a
subjective psychological assessment.
Common coccydynia
is related to coccygeal instability in almost half of the cases. The diagnosis
should be documented with dynamic X-ray films to evidence luxations and
hypermobility, wich may need specific treatments. Spicules, which account for
15% of the cases are also easy to diagnose. Treatment of common coccydynia
should be considered according to this diagnosis.
 References
References
· Gray H 1973 Gray's Anatomy, 35th ed. Longman, Edinburgh
· Howorth B 1959 The painful coccyx. Clinical Orthopedics 14:145-150
· Jurmand SH 1976 Les injections péridurales dans le traitement de la
coccygodynie. Rev Rhum 43: 217-220
· Maigne JY 1992 Coccygodynie: intérêt des clichés dynamiques. Revue du
Rhumatisme et des Maladies Ostéoarticulaires
· Maigne JY, Guedj S, Straus C. Idiopathic Coccygodynia : Lateral Roentgenograms
in the Sitting Position and Coccygeal Discography. Spine 1994;19:930-4
· Maigne JY, Molinie V, Fautrel B. 1992 Anatomie des disques coccygiens. Revue
de Medecine Orthopedique. 28:34-35
· Maigne JY 1996 Standardized Radiological Protocol for the Study of Common
Coccydynia. Characteristics of the Lesions Observed in the Sitting Position.
Clinical Elements Differentiating Luxation, Hypermobility and Normal Mobility.
Spine, 1996;22:2588-93
· Maigne R 1961 Les manipulations vertébrales. 3rd ed. Paris: Expansion
Scientifique Française:180
· Nelson DA 1991 Idiopathic coccygodynia and lumbar disk disease: Historical
correlations and clinical cautions. Perspectives in Biology and Medicine 34:
229-238
· Postacchini F, Massobrio M 1983 Idiopathic coccygodynia: analysis of fifty-one
operative cases and a radiographic study of the normal coccyx. Journal of Bone
and Joint Surgery 65A: 1116-1124
· Pyper JB 1957 Excision of the coccyx for idiopathic coccygodynia. Journal of
Bone and Joint Surgery 39B: 733-737
· Saluja PG 1988 The incidence of ossification of the sacrococcygeal joint.
Journal of Anatomy156:11-15
· Stern FH 1967 Idiopathic coccygodynia among the geriatric population. Journal
of the American Geriatric Society 15: 100-102
· Smout CF, Jacoby F, Lillie EW 1969 Gynaecological and Obstetrical Anatomy,
12th edn. Oxford University Press, Oxford
· Thiele GH 1937 Coccydynia and pain in the superior gluteal region. JAMA
109:1271–5
· Wray CC, Easom S, Hoskinson J. Coccydynia 1991 J Bone Joint Surg [Br]
73-B:335-8
|
